- BMH Group
- Our Hospitals
-
Our Specialities
- Cardiology
- Orthopaedic And Arthroscopic Surgery
- Neurology
- Neurosurgery
- Spine Surgery
- Urology
- Surgical Gastroenterology
- Medical Gastroenterology And GI Endoscopy
- Joint Replacement
- General And Laparoscopic Surgery
- Advanced Robotic And Laser Urology
- Anaesthesiology
- Audiology
- Paediatrics And Neonatology
- Cardiac Anaesthesiology
- Cardiac Electrophysiology
- Cardiovascular Thoracic Surgery
- Clinical Psychology
- Cranio Maxillofacial Surgery
- Critical Care Medicine
- Dental
- Dermatology And Cosmetology
- Dietetics
- Emergency Medicine
- Endocrine Surgery
- Endocrinology
- Endodentics
- ENT And Head & Neck Surgery
- Family Medicine
- Foetal Medicine
- Haematology, Haemato-Oncology And BMT
- Infectious Diseases
- Infertility And Reproductive Medicine
- Interventional Radiology
- Internal Medicine
- Kidney Transplant
- Liver And HPB Surgery
- Liver Transplant
- Medical Oncology
- Nephrology
- Neurointervention And Neuroradiology
- Nuclear Medicine
- Obstetrics And Gynaecology
- Ophthalmology
- Paediatric Cardiology
- Paediatric Orthopaedics
- Paediatric Surgery
- Physical Medicine And Rehabilitation
- Physiotherapy
- Plastic, Aesthetic And Reconstructive Surgery
- Preventive Medicine And Wellness
- Psychiatry
- Pulmonology
- Radiation Oncology
- Radiology And Clinical Imaging
- Rheumatology And Clinical Immunology
- Sports Medicine
- Surgical Oncology
- Vascular Surgery View All
- Our Doctors
-
Treatments
- Robotic Total Knee Replacement
- Total Knee Replacement (TKR)
- Transurethral Resection of the Prostate (TURP)
- Skin Grafting
- Stroke Management
- Holter Monitoring
- Coronary Angioplasty and Stenting (PTCA)
- Pacemaker Implantation
- Electrophysiology Study (EPS)
- Balloon Valvuloplasty
- Neuromuscular Disorders Management
- Peripheral Angioplasty
- Burn Surgery & Scar Management
- Heart Failure Management
- Epilepsy Management
- Headache and Migraine Management
- Multiple Sclerosis (MS) Management
- Dementia and Memory Disorders Management
- Microvascular Surgery
- Hand Surgery
- Nerve Conduction Studies (NCS) and Electromyography (EMG)
- Botox Therapy for Neurological Conditions
- Parkinson’s Disease and Movement Disorders Management
- Autoimmune Neurological Disease Management
- Breast Reconstruction
- Heart Valve Replacement Surgery
- Brain Tumor Surgery
- Cleft Lip And Palate Repair
- Sigmoidoscopy with Polypectomy
- Aneurysm Clipping And Coiling
- Traumatic Brain Injury (TBI) Management
- Cerebrovascular Accident (Stroke) Management
- Non-Surgical Cosmetic Procedures
- VP Shunt Placement
- Endoscopic Neurosurgery
- Peripheral Nerve Surgery
- Epilepsy Surgery
- Cataract Surgery
- Functional Neurosurgery
- Spine Tumor Surgery
- Glaucoma Management
- Cardiac Rehabilitation
- Diabetic Retinopathy
- Reconstructive Surgery
- Oculoplastic Surgery
- ERCP
- Upper GI Endoscopy
- Colonoscopy
- ACL Reconstruction
- Robotic Radical Prostatectomy
- Coronary Artery Bypass Grafting (CABG)
- Therapeutic Plasma Exchange
- TAVI/TAVR
- Spinal Deformity Correction
- Laser Lithotripsy for Kidney Stones
- Facial Aesthetic Surgeries
- Lumbar Disc Herniation Repair
- Breast Surgery
- Transcatheter Closure of Septal Defects
- Body Contouring
- Dialectical Behavior Therapy
- Robotic Assisted Cardiothoracic Surgery
- Flap Surgery
- Liver Resection
- Hair Restoration
- Cognitive Behavioral Therapy (CBT)
- Bronchoscopy
- Spinal Fusion Surgery
- Sleep Study (Polysomnography)
- Microdiscectomy
- Hernia and Abdominal Wall Surgeries
- Whipple’s Surgery
- Labral Tear Repair (Shoulder or Hip)
- COPD Management
- Laparoscopic Hernia Repair
- Laparoscopic Colorectal Surgery
- Adenoidectomy
- Stapedotomy
- Tympanoplasty
- Pulmonary Rehabilitation
- Kidney Transplant
- Interstitial Lung Disease (ILD) Treatment
- Parathyroidectomy
- Lung Infection Management
- Tumour Embolisation
- Liver Transplant (Deceased Donor)
- Meniscus Repair
- Laparoscopic Hysterectomy
- Asthma and Allergy Management
- Composite Filling
- Cholangioscopy
- Minimally Invasive Endocrine Surgeries
- Hemoperfusion
- Robotic Prostate Surgery (Robotic Prostatectomy)
- Total Hip Replacement (THR)
- Neuro Rehabilitation
- Cerebral Angiography
- Pain Management And Musculoskeletal Rehabilitation
- Spinal Angiography
- Endoscopic Ultrasound (EUS)
- Amputee And Prosthetic Rehabilitation
- Septoplasty
- Uterine Artery Embolisation (UAE)
- Adrenalectomy
- Laparoscopic Cholecystectomy
- Liver Transplant (Living Donor)
- Paediatric Liver Transplant
- Cochlear Implant
- Carotid Artery Stenting
- Pancreatic Necrosectomy
- Transarterial Chemoembolisation (TACE)
- Continuous Renal Replacement Therapy (CRRT)
- Root Canal Treatment
- High-Risk Pregnancy Management
- Rotator Cuff Repair
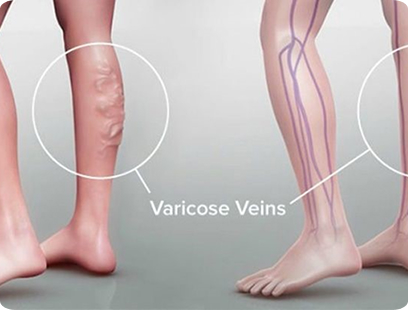
- Varicose Vein Ablation
- Colon Polypectomy
- Solution-Focused Brief Therapy
- Pancreatic Endocrine Tumor Resection
- Ablation for Arrhythmias
- RIRS (Retrograde Intrarenal Surgery)
- PRP
- Microneedling
- Allergy Immunotherapy
- Chemical Peeling
- Bariatric Surgery
- Functional Endoscopic Sinus Surgery (FESS)
- Radioiodine Therapy
- External Beam Radiation Therapy
- Thyroidectomy
- Aortic Aneurysm Repair
- Chronic Kidney Disease (CKD) Management
- Acute Kidney Injury (AKI) Treatment
- Percutaneous Endoscopic Gastrostomy
- Robotic Gynaecologic Surgery
- Hemodialysis
- Minimally Invasive Cardiac Surgery
- Diabetes Care
- Brachytherapy
- Peripheral Vascular Bypass Surgery
- Peritoneal Dialysis
- Kidney Biopsy
- Beating Heart Bypass Surgery
- Diabetic Nephropathy
- Awake Cardiac Surgery
- Anemia Management in CKD
- Chronic Ambulatory Peritoneal Dialysis
- Targeted Therapy
- Chemotherapy View All
- LifeLinER
- Academics & Research
- International patients
- Career
- Contact Us